



Categories: Peptide Finished product, Peptides and Their Dosages
Free (1) 30 ml Bacteriostatic Water
with qualified orders over $500 USD.
(excludes capsule products, cosmetic peptides, promo codes and shipping)
KPV is a potent anti-inflammatory peptide that has shown promise in a number of disease conditions. The most active research is in the treatment of inflammatory bowel disease where the peptide has showed substantial promise. KPV has been shown in animal studies to be safe and effective when administered orally, intravenously, subcutaneously and transdermal. Research in wound healing also reveals that KPV and other alpha-MSH derivatives may offer a host of benefits that speed wound healing, reduce infection, fight inflammation, and lead to better cosmetic results. KPV and similar peptides could become mainstays not just in wound healing, but in scar reduction following surgery.
Product Usage: This PRODUCT IS INTENDED AS A RESEARCH CHEMICAL ONLY. This designation allows the use of research chemicals strictly for in vitro testing and laboratory experimentation only. All product information available on this website is for educational purposes only. Bodily introduction of any kind into humans or animals is strictly forbidden by law. This product should only be handled by licensed, qualified professionals. This product is not a drug, food, or cosmetic and may not be misbranded, misused or mislabled as a drug, food or cosmetic.
KPV is the C-terminal peptide fragment of alpha-melanocyte stimulating hormone (alpha-MSH). It is one of many short peptide derivatives of alpha-MSH that has been tested to determine if they retain similar photoprotective properties, activity against ischemia, sexual effects, or benefits on feeding behavior and energy homeostasis. KPV, which is made up of lysine-proline-valine turns out to have significant anti-inflammatory effects[1]. The peptide is under active research as a potential therapeutic in the treatment of inflammatory bowel disease. It has shown evidence of potent anti-inflammatory activity in the central nervous system, GI tract, lungs, vascular system, and joints. Because KPV is a small peptide, it can be administered in multiple ways including oral, intravenous, and transdermal routes.
Perhaps the most important discovery to arise from KPV research is the finding that the peptide reduces intestinal inflammation. In mouse models of inflammatory bowel disease (IBD), KPV shows robust results, reducing inflammatory infiltrates, MPO activity, and overall histological evidence of inflammation. Mice treated with KPV in the study recovered faster and had more pronounced weight gain than mice treated with placebo[2].
Further research on delivery mechanisms for KPV has revealed that loading KPV onto nanoparticles functionalized with hyaluronic acid helps to direct the inflammatory effects of the peptide to proper locations within the intestine. This leads to accelerated mucosal healing and alleviation of inflammation via a strong down regulation of TNF-alpha in mouse models[3]. In many ways, KPV is a more effective and more targeted means of reducing inflammation in IBD without affecting TNF-alpha in other locations in the body. The benefit of modifying KPV is in improving the peptide’s oral bioavailability. This does not increase the efficacy of the peptide, but does have an impact on potency and thus total dose require to achieve an effect.
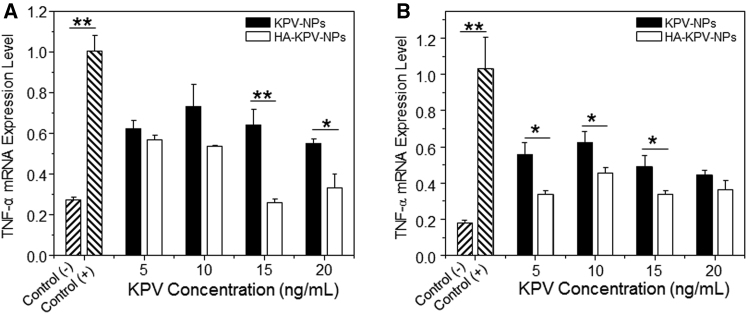
Research suggests that TNF-alpha is not the only inflammatory mediator that KPV has an impact on. The peptide also reduces NF-kappaB and mitogen-activated protein kinase activity. These effects work in tandem with TNF-alpha inhibition to reduce inflammatory changes in the intestine. Mice treated with KPV have substantially less colonic infiltration and normal colon lengths compared to controls[4].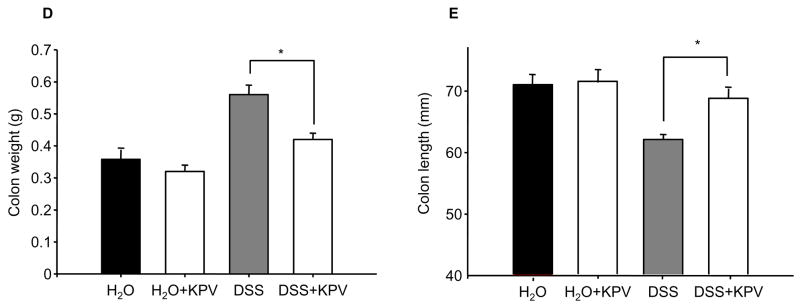
Source: PubChem
Of interest in the graph above is the fact KPV appears to only have an effect in the setting of overblown inflammation. It has almost no effect in normal tissue. At least part of the reason for this is that KPV enters colonic cells via a transporter that is unregulated in the setting of inflammation. This suggests that KPV may be an effective preventative or maintenance medication in the setting of IBD. It can be safely taken even during quiescent periods because it has no effect. It taken regularly, then the peptide will be available when needed and simply excreted otherwise. Professor Didier Merlin, who has led a great deal of research into the potential GI benefits of KPV, has recently found that the peptide enters colonic cells via PepT1, a protein channel that is only expressed in any real quantity in the intestine during inflammatory states. This helps to explain why KPV is more effective in already inflamed settings. It also suggests a new mode of drug delivery that could be applicable to a number of conditions. By targeting proteins that are altered in disease conditions, even if they are not directly pathogenic, it may be possible to concentrate the activity of drugs in certain areas. This could allow for decreased dosing of drugs with serious side effects and the development of drugs that, while not potent on their own, are formidable therapeutics in the setting of the right disease state.
As far back as 1984, research in rabbits revealed that KPV is a powerful anti-inflammatory and fever reducer (anti-pyretic). In this setting, however, KPV had lower potency than the full alpha-MSH molecule. This suggested to scientists at the time that KPV was lacking some portion of the alpha-MSH molecule necessary for full anti-pyretic activity[5]. What ensued was decades of research investigating various modified forms of alpha-MSH.
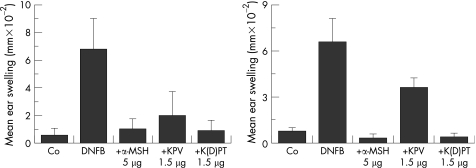
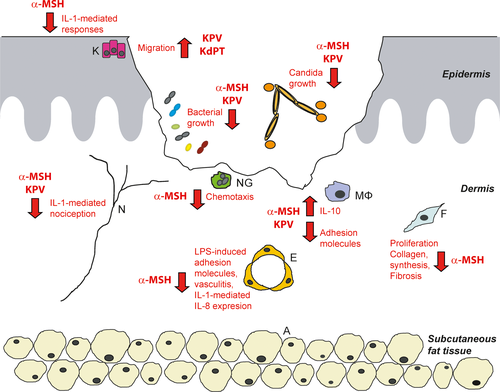
Perhaps the biggest lesson learned from these tests is that alpha-MSH and several of its analogues all reduce inflammation in a wide variety of disease. So far, the molecules have been tested in fever, irritant and allergic contact dermatitis, vasculitis, fibrosis, arthritis and inflammation of the eyes, brain, lungs, and gastrointestinal tract. In all cases, alpha-MSH is the most effective anti-inflammatory. Unfortunately, it suffers from one major side effect – it causes skin pigmentation. KPV, on the other hand, does not have this side effect. And even though KPV is not as potent as the intact alpha-MSH, its lack of side effects means that boosting levels to achieve desired target effects is theoretically possible in most cases[6].
The difference in potency has been found to be minimal, at best, as the majority of anti-inflammatory effects of alpha-MSH are, in fact, due to the KPV section. What is interesting, however, is that the parent molecule appears to be better at suppressing late-stage inflammatory reaction. In the case of contact dermatitis, for instance, alpha-MSH does a better job of preventing an allergic inflammatory response at 2 weeks post initial exposure. This suggests that alpha-MSH may be affecting some aspect of immune modulation that is separate from the immediate inflammatory response[7]. Work is still being done to determine what this process is.
Graph shows ear swelling due to contact dermatitis at 24 hours (left) and 2 weeks (right). Note that co-administration of KPV with the irritant is nearly as effective as co-administration of alpha-MSH with the irritant at 24 hours. At 2 weeks, however, exposure to the stimulus without co-administration of the peptides shows much less swelling with alpha-MSH compared to KPV.
Wound healing is a complex physiological process. Scientists have identified three general phases in the wound healing process: inflammatory, proliferative, and remodeling. Each phase is characterized by differences in cell populations and cytokine concentrations and represents a unique chemical/physiological milieu for potential intervention. Research shows that even though each stage of the wound healing process is characterized by different skin cell subtypes, the majority of these cells express a melanocortin 1 receptor (MC1R) that binds alpha-melanocyte-stimulating hormone. Of course, this also means that these cells types bind alpha-MSH analogues like KPV and KdPT as well[6].
Because these alpha-MSH derivatives retain some of the properties of alpha-MSH, but lack others, they offer potential benefits in wound healing. For instance, KPV offers the inflammatory properties of alpha-MSH, but lacks the pigment-inducing activity of its parent peptide. This makes KPV a good candidate for improving wound healing while avoiding the skin-changing characteristics often associated with natural scar formation (a phenomenon disproportionately affecting darker-skinned individuals).
One of the reasons that KPV is anti-inflammatory is that it participates in the innate immune response against two common skin pathogens. Research shows that KPV inhibits the growth of both Staphylococcus aureus and Candida albicans. These benefits occur at physiological concentrations, meaning that KPV could provide an effective means of preventing infection in the setting of serious wounds like burns. This benefit of KPV is in contrast to other anti-inflammatory medications that actually inhibit the ability of the body to fight off infection. Thus, KPV combines anti-inflammatory activity with antimicrobial activity[8].
KPV actually serves as a structural model in recent research looking to replicate the anti-fungal effects of the peptide in novel therapeutics. The idea is that the 3D structure of KPV is what makes it an effective anti-fungal and that replicating this structure could allow researchers to develop compounds that have the same anti-fungal activity but different effects on other biological processes[9].
In accordance with the known benefits of KPV in first stage (inflammation) of wound healing, research has also investigated its role in the other two stages of wound healing. It appears that KPV is able to reduce the kind of chronic inflammation that leads to hypertrophic scar (e.g., keloid) formation. This type of scarring is characterized by widespread macrophage infiltration, TNF immunoreactivity, and neutrophil abundance. Administration of alpha-MSH in this setting leads to smaller scars and a less drastic inflammatory response[10]. Similar effects have been noted in other tissues such as lung and heart. These findings raise the hope that KPV could be useful in preventing the kind of scarring seen with certain chemotherapy agents[11]–[13]. This would not only reduce the side effects of cancer treatment, but could allow for the use of increased concentrations of these medications and thus better outcomes in cancer treatment.
According to Dr. Didier Merlin, at least part of the benefit of KPV in reducing scar prominence appears to arise from its ability to modulate collagen metabolism. Alpha-MSH and its analogues suppress IL-8 secretion, which inhibits collagen type 1 production. This is important during the last phase of wound healing, remodeling, as it has been shown that people prone to keloid formation and hypertrophic scarring have less MC1R mRNA expression on dermal fibroblasts[14].
While alpha-MSH is the more potent molecule of the two, it has one serious disadvantage when compared to KPV – it causes skin pigmentation. This side effect alone has been enough to discourage further research into intact alpha-MSH as a potential anti-inflammatory. KPV is favored because it retains most of the anti-inflammatory properties of alpha-MSH yet has none of the side effects. KPV is also exceptionally easy to manufacture and thus has benefit from a cost and logistics standpoint as well[15]. Dr. Thomas Luger, a renowned dermatologist and expert in inflammatory diseases of the skin, has published on KPV extensively. His work demonstrates that the peptide has potent anti-inflammatory properties with few adverse effects.
It is also important to note that the anti-inflammatory effects of KPV appear to be mediated through a different mechanism than those of alpha-MSH. Whereas alpha-MSH binds to specific melanocortin receptors, KPV does not. Evidence of this comes from mouse studies in which blocking MC3/4 receptors, which mediate the anti-inflammatory effects of alpha-MSH, has no impact on the anti-inflammatory effects of KPV. Specifically, blocking these receptors does not block the leukocyte migration effects induced by KPV[16].
Another appealing aspect of KPV is the ease with which the peptide can be administered. Research in animal models has shown that KPV can be administered both orally, subcutaneously and via injection (peripherally or centrally) without serious side effects. Recently, similar research showed that KPV could be administered trans-dermally with success[17]. The ability to administer the drug via multiple routes is not just a matter of convenience either. Different routes of administration affect the way the peptide works and where its anti-inflammatory effects are targeted. The ability to alter the method of delivery makes it possible for scientists to target different areas within the body for treatment.
KPV is a potent anti-inflammatory peptide that has shown promise in a number of disease conditions. The most active research is in the treatment of inflammatory bowel disease where the peptide has showed substantial promise. KPV has been shown in animal studies to be safe and effective when administered orally, intravenously, subcutaneously and through the skin. Research in wound healing also reveals that KPV and other alpha-MSH derivatives may offer a host of benefits that speed wound healing, reduce infection, fight inflammation, and lead to better cosmetic results. KPV and similar peptides could become mainstays not just in wound healing, but in scar reduction following surgery.
KPV exhibits minimal side effects, low oral and excellent subcutaneous bioavailability in mice. Per kg dosage in mice does not scale to humans. KPV for sale at
PeptideGurus is a leading supplier of American-made research peptides, offering top-quality products at competitive prices. With a focus on excellence and customer service, they ensure a secure and convenient ordering process with global shipping.
CONTACT